Exploring the link between hearing loss, dementia & Alzheimer’s Disease
Search for articles by category
Introduction
Untreated hearing loss goes beyond mere auditory decline; it encompasses a myriad of adverse effects that can significantly impact overall health and well-being 1. Studies 2,3,4, 5,6 have established an association between hearing loss and various health issues, including dementia and Alzheimer's disease. Both conditions, hearing loss and dementia, are prevalent among older adults, with an estimated 57 million people worldwide diagnosed with dementia 7.
Understanding Dementia and Alzheimer’s Disease
Alzheimer’s disease is a progressive brain disorder, representing the primary cause of dementia. Dementia itself isn't a distinct ailment but rather an umbrella term for a collection of symptoms. Initial indicators of Alzheimer’s include lapses in recent memories or conversations, evolving into profound memory impairment and an inability to carry out daily tasks 8.
The global impact of Dementia
The global number of people with Alzheimer's disease (AD) dementia, prodromal Alzheimer's disease, and preclinical Alzheimer's disease were estimated at 32 million, 69 million, and 315 million, respectively. Together, these groups totaled 416 million individuals across the Alzheimer's disease continuum, representing 22% of all people aged 50 and above 9. In the United States alone, approximately 6.5 million individuals aged 65 and older grapple with Alzheimer's disease, with over 70% of cases occurring in those aged 75 and older. Globally, of the approximately 57 million people affected by dementia, 60% to 70% are believed to have Alzheimer's disease. Without medical advancements, the number of cases is expected to double every 20 years, reaching a staggering 139 million cases by 2050 10. This surge in dementia cases will contribute to approximately 115.8 million disability-adjusted life years 7.
Link between hearing loss and cognitive decline
The association between hearing loss and cognitive decline is significant, as hearing loss can lead to reduced auditory input and social isolation, both of which negatively impact cognitive function. Furthermore, hearing loss has been linked to an increased risk of dementia and Alzheimer's disease, potentially due to the additional cognitive load required to process sound and the resulting brain changes. Given these connections, the research evidence emphasizes the importance of early detection and management of hearing loss to mitigate its potential implications on cognitive health and help address the rising number of dementia cases.
Significance of early hearing loss detection and management
A global commission examining dementia care and prevention identified a dozen pivotal risk factors, selected for their significant impact and potential modifiability. The elimination of these 12 factors could potentially prevent up to 40% of dementia cases 11. Among these factors, untreated hearing loss emerges as a significant contributor. Hearing loss, affecting 10% of individuals aged 40–69, 30% of those over 65, and up to 90% in those aged 85 years or older, contributes to an estimated 8% of dementia cases worldwide. This translates to approximately 4 million of the 57 million dementia cases worldwide being linked to untreated hearing loss.
Hearing loss affects nearly two-thirds of those over 70 years old. Combined with a significantly heightened risk of dementia, individuals with untreated hearing loss are 90% more likely to develop dementia compared to those with normal hearing. In comparison, other risk factors such as hypertension only confer a 60% increased risk of dementia, while comparable risk factors, such as hypertension, only confer a 60% increased risk of dementia.
The impact of managing hearing loss could be profound, potentially preventing up to 8% of dementia cases globally. This emphasizes hearing loss as the most substantial contributor to dementia risk. Research indicates that even mild hearing impairment elevates the risk of long-term cognitive decline and the development of dementia. This growing understanding of the association between hearing loss and dementia has prompted increased public health attention, offering valuable insights for the development of early detection tools and effective interventions.
Physiological connections
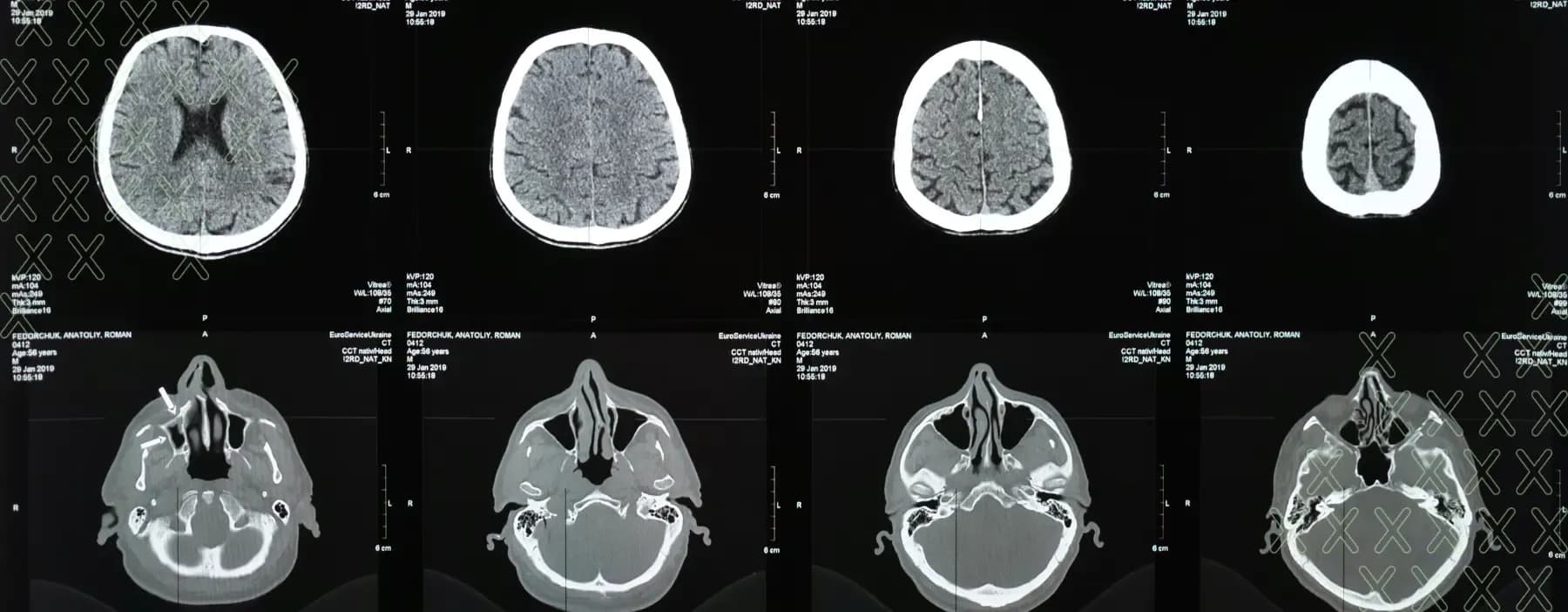
Shared physiological alterations observed in both the ear and the brain cortex hint at a potential connection between hearing loss and dementia. Studies indicate that individuals with Alzheimer’s disease often exhibit changes in the cochlea, a vital component of hearing, as well as in nuclei within the ascending auditory pathway. Additionally, changes may be detected in the auditory cortex of the brain. In cases of vascular dementia, damage to blood vessels may adversely affect the auditory structures.
Individuals experiencing hearing loss encounter diminished auditory input, resulting in potential missed verbal and emotional cues crucial for social interactions. The absence of such vital information can directly impact brain structure and function, potentially impeding cognitive processes. Diminished social interactions, similar to risk factors like smoking and physical inactivity, may heighten the risk of dementia.
Cognitive burden and listening fatigue
Hearing loss imposes a cognitive burden as individuals exert additional cognitive resources to decipher auditory stimuli, known as “listening fatigue”. This allocation of cognitive energy may detract from other cognitive processes such as memory, language processing, and attention. The strain of comprehension, especially in noisy environments, could precipitate a decline in various brain functions, reminiscent of dementia symptoms.
Researchers suggest that anatomical changes to the brain's medial temporal lobe (MTL) may be associated with the development of Alzheimer’s disease 12. Individuals with Alzheimer’s disease often exhibit abnormal accumulations of tau protein, forming neurofibrillary tangles within neurons, alongside excess beta-amyloid 42, leading to plaque formation. These neuronal changes are observed first in the MTL, implicating its role in auditory processing. Individuals with hearing loss also demonstrate MTL neuronal changes, suggesting an interplay between the two conditions.
Limited auditory input may trigger MTL overactivity, potentially contributing to neurofibrillary tangles and beta-amyloid plaques. Moreover, the relationship between hearing loss and Alzheimer’s disease may be bidirectional, exacerbating each other’s effects.
Furthermore, regular mental stimulation and social engagement are known to bolster cognitive reserve, the brain’s ability to withstand challenges, including dementia-related diseases. Hearing loss may impair an individual's capacity to build and safeguard their cognitive reserve, potentially elevating dementia risk. Understanding the comprehensive impact of hearing loss on the quality of life for older adults extends beyond mere communication challenges, necessitating awareness among general practitioners and empowering older individuals with knowledge about their hearing health13 . Such awareness may foster compliance with broader hearing and medical rehabilitation recommendations.
Implications for public health
Early detection of hearing loss and subsequent aural rehabilitation can yield significant long-term benefits for quality of life and mental well-being. A growing body of epidemiological evidence 14 corroborates what many Audiologists have observed clinically for decades: hearing loss exerts a profound influence on various facets of life, including heightened social isolation, increased risk of depression, and diminished physical activity or social engagement—each contributing independently to the risk of dementia. While causality between hearing loss and dementia remains to be definitively established, emerging studies suggest its plausibility, highlighting the potential far-reaching advantages of hearing loss management.
Routine hearing assessments play a pivotal role in hearing conservation and the early detection of conditions associated with hearing loss. Digital audiometry solutions like hearTest offer convenient access to and implementation of hearing conservation programs. By facilitating extended high-frequency monitoring, hearTest can detect early signs of hearing loss before they impact speech frequencies, thus pre-empting the onset of communication difficulties and adverse effects of hearing loss, so that lifestyle changes can be made to prevent the further deterioration of hearing. Additionally, hearTest provides hearing threshold results crucial for programming hearing aids tailored to address hearing loss.
Current research and future directions
Research highlights the positive association between hearing aid usage and enhanced cognitive function, suggesting that hearing aids not only improve hearing but also mitigate cognitive decline. As such, prioritizing regular hearing checks and embracing hearing aid technology can significantly contribute to maintaining cognitive health and overall well-being. As researchers strive to understand the complexities of Alzheimer’s disease, ongoing studies are dedicated to exploring novel interventions and treatments. Given the multifaceted nature of the disease and the myriad factors contributing to its risk, current research is focused on various fronts.
Numerous drugs and medical devices in development target key brain changes associated with Alzheimer’s, offering potential avenues to impede disease progression. These changes, including the accumulation of beta-amyloid and tau proteins, neuroinflammation, immune response modulation, and metabolic alterations, serve as promising targets for therapeutic interventions. Experts anticipate that future treatments will likely involve a multifaceted approach, incorporating medications or devices targeting multiple disease-related mechanisms, akin to treatment strategies employed in managing cancers and AIDS.
Practical recommendations
Looking ahead, the landscape of hearing healthcare is poised for significant transformation as research continues to advance, and policy changes reshape care models and accessibility to hearing services. The involvement of hearing care providers, alongside family members and caregivers, holds profound implications for older adults with hearing loss, influencing both their well-being and overall health outcomes.
Conclusion
Engaging patients in ongoing discussions regarding their communication needs, as well as broader health and disease prevention strategies, stands to enhance collective efforts in promoting the longevity and vitality of older adults. Recognizing the impact of hearing loss on overall health and integrating aural rehabilitation into comprehensive health initiatives across medical specialties and primary care settings can foster stronger patient-provider connections and better support older adults as they navigate their later years. Through collaborative efforts and a holistic approach to care, we can empower older adults to lead fuller, healthier lives.



